This is for POWH Medical Services

Clinical Psychology Department
We offer psychological support as part of treatment and rehabilitation plans and can help you adjust to your injury or illness. This is available to you if you are a patient in the Aged Care, Spinal or the General Rehabilitation wards.
We do this by:
- Assessing your psychological and cognitive abilities
- Assessing your capacity to make decisions
- Offering treatments for a wide variety of psychological problems
- Offering psychological support to family members
- Providing psychological education and information to patients and their families
- Working with the other health professionals on your health care team to develop your treatment plan while you are in hospital and to help develop a plan for when you go home.
We also offer a limited outpatient service as part of the Cognitive Disorders Clinic.
Manager
Head of Department. Alison Grundy, Senior Clinical Psychologist
How to find us
Level 1, High Street Building opposite the Occupational Therapy gym. (Building 2B on our campus map)
We are a team of registered Clinical Psychologists and Clinical Neuropsychologists who offer assessments and treatments across a wide variety of psychological and cognitive issues.
- Clinical Psychologists offer assessment and treatment of psychological conditions such as adjustment to illness or injury, trauma, depression and anxiety.
- Clinical Neuropsychologists offer assessment and rehabilitation of cognitive conditions such as dementia, brain injury and stroke.
Our primary partners are the other members of your health care team especially those within the rehabilitation wards. When planning for your return home we work in partnership with your local general practitioner (GP), Prince of Wales Hospital and Community Health Services, non- government rehabilitation and support services and private community psychologists.
As an inpatient of the Aged Care, Spinal or General Rehabilitation wards, you can ask your nurse or any member of your treating team to make an appointment with a psychologist.
When you see one of our team we will explain what assessments or treatments we can offer you and we will ask for your consent before proceeding with any treatments. Psychologists use a wide range of assessment and treatment protocols to help people adjust to their injuries, deal with such issues as anxiety and depression, cope with declining memory and mental functioning and support your in-patient stay and rehabilitation.
Please let us know if you need an interpreter. You can contact us telephoning the Translating and Interpreting Service (TIS) on 131 450. Tell the operator what language you speak and then ask the interpreter to set up a telephone conversation between you, an interpreter, and the healthcare professional you want to speak with.
We are a teaching hospital and you may be asked to be involved in research or a student to be present at your appointment. You have a right to say no. If you do so, this will no impact in any way on the services we will provide.
Neurology services and clinics
How we can help you?
A neurologist is a medical specialist who assesses, diagnoses and treats problems with your brain, nerves and muscles. The problems may range from headache and pain, dizziness and imbalance, to problems with feeling, strength and balance.
Our services include:
- an inpatient Neurosciences Ward (Level 8 North and South, Acute Services Building, Prince of Wales Hospital). This ward also cares for patients who have experienced stroke.
- a neurophysiology laboratory which can do a range of tests to help in the assessment and diagnosis of nervous system disorders
- multiple clinics which specialise in different nervous system problems.
Managers
Head of Department of Neurology Prof James Colebatch
Our contact details
Department of Neurological Sciences:
Phone: (02) 9382 2414
Level 2, High St building, Prince of Wales Hospital (Building 2 on our campus map)
Neurosciences ward:
Phone: (02) 9382 9800
Location: Level 8 North and South, Acute Services Building, Prince of Wales Hospital (Building 30 on our campus map)
We care for people who have a diagnosis of nervous system disorders who do not require surgical treatment. We have speciality clinics to support patients requiring investigation for stroke, epilepsy and neuromuscular disorders.
We also have a general neurology clinic for those patients who don't meet the criteria for the speciality clinics. This clinic is for patients living within the local area surrounding Prince of Wales Hospital. It is for review and management of conditions such as headaches, vertigo or memory issues.
All our clinics require a referral prior to you to making an appointment.
Clinic Name |
What it does |
Time and Date |
Telephone |
Consultants |
|
Nerve and Muscle Clinic |
Disease of peripheral nervous system |
Fortnightly |
9382 2422 |
Prof A Krishnan, Dr J. Offord, Dr D Dhanapalaratnam |
|
Epilepsy clinic |
Comprehensive management of epilepsy patients |
Weekly |
9382 3805 |
Prof E. Somerville, Dr H. Laue-Gizzi, Dr C. Zentner, Dr P. Gordon, Dr D Ghougassian, Epilepsy Fellows |
|
First seizure clinic |
First seizure management |
Weekly |
9382 3805 |
Prof E. Somerville, Dr H. Laue-Gizzi, Dr C Zentner, Dr P. Gordon, Dr D Ghougassian, Epilepsy Fellows |
|
Neurophysiology clinic |
EEG, EMG, EP, Vestibular testing |
Daily |
9382 2211 |
Multiple reporting doctors |
|
Multiple sclerosis clinic |
Inflammatory CNS disorders |
Weekly |
9382 2414 |
Prof A. Krishnan |
|
General neurology clinic |
General neurological problems |
Three times a week |
9382 2407, 9382 2422, 9382 2414 |
Profs J Colebatch, A Zagami, A Krishnan, Dr J. Offord, Dr D Dhanapalaratnam |
|
Private clinics |
General neurological problems |
Three times a week |
9382 2407, 9382 2422 |
Profs J Colebatch, A Zagami |
For more information, please see our links on the right hand side of this page.
You need a referral letter from your local general practitioner (GP) or medical practitioner to access this service.
Your doctor will need to fax your referral letter to us to the appropriate fax number. If there is a waiting list, you will receive a confirmation letter and be told what to do next. If there is no waiting list, you will receive a letter providing details on the time and date of your appointment booking or we will contact you to arrange a suitable time. You may receive an SMS or telephone reminder prior to your appointment.
If you need to change or cancel your appointment please telephone the relevant number in our list of clinics. This will allow us to make the time available to another patient.
Please bring:
- Your appointment letter
- Any special items listed on your letter
- TAC or Workcover claim number (if relevant)
- Medicare card
- Health Care Card and/or concession card
- Private health insurance card
- Adverse drug alert card
- Previous x-ray films, scans, ultrasounds or any other test results or reports relevant to your current condition
- Medicines you need to take while you are here
- List of medicines you are currently taking (or the boxes), including medicines you have bought without a prescription, such as herbal supplements and vitamins
- Glasses, hearing aid, walking frame
If you are having a day procedure, please bring:
- Responsible adult carer to stay with you to hear instructions, help you and take you home
- Comfortable day clothes, such as a tracksuit
Please let us know if you need an interpreter. You can contact us telephoning the Translating and Interpreting Service (TIS) on 131 450. Tell the operator what language you speak and then ask the interpreter to set up a telephone conversation between you, an interpreter, and the healthcare professional you want to speak with.
We are teaching hospital and you may be asked to have students present at your appointment or to be involved in research. You have a right to say no. If you do so, this will may cause a slight delay but will not impact on the services we will provide. You may be seen by a senior registrar or Fellow.
Neurology services and clinics
How we can help you?
A neurologist is a medical specialist who assesses, diagnoses and treats problems with your brain, nerves and muscles. The problems may range from headache and pain, dizziness and imbalance, to problems with feeling, strength and balance.
Our services include:
- an inpatient Neurosciences Ward (Level 8 North and South, Acute Services Building, Prince of Wales Hospital). This ward also cares for patients who have experienced stroke.
- a neurophysiology laboratory which can do a range of tests to help in the assessment and diagnosis of nervous system disorders
- multiple clinics which specialise in different nervous system problems.
Managers
Head of Department of Neurology Prof James Colebatch
Our contact details
Department of Neurological Sciences:
Phone: (02) 9382 2414
Level 2, High St building, Prince of Wales Hospital (Building 2 on our campus map)
Neurosciences ward:
Phone: (02) 9382 9800
Location: Level 8 North and South, Acute Services Building, Prince of Wales Hospital (Building 30 on our campus map)
We care for people who have a diagnosis of nervous system disorders who do not require surgical treatment. We have speciality clinics to support patients requiring investigation for stroke, epilepsy and neuromuscular disorders.
We also have a general neurology clinic for those patients who don't meet the criteria for the speciality clinics. This clinic is for patients living within the local area surrounding Prince of Wales Hospital. It is for review and management of conditions such as headaches, vertigo or memory issues.
All our clinics require a referral prior to you to making an appointment.
Clinic Name |
What it does |
Time and Date |
Telephone |
Consultants |
|
Nerve and Muscle Clinic |
Disease of peripheral nervous system |
Fortnightly |
9382 2422 |
Prof A Krishnan, Dr J. Offord, Dr D Dhanapalaratnam |
|
Epilepsy clinic |
Comprehensive management of epilepsy patients |
Weekly |
9382 3805 |
Prof E. Somerville, Dr H. Laue-Gizzi, Dr C. Zentner, Dr P. Gordon, Dr D Ghougassian, Epilepsy Fellows |
|
First seizure clinic |
First seizure management |
Weekly |
9382 3805 |
Prof E. Somerville, Dr H. Laue-Gizzi, Dr C Zentner, Dr P. Gordon, Dr D Ghougassian, Epilepsy Fellows |
|
Neurophysiology clinic |
EEG, EMG, EP, Vestibular testing |
Daily |
9382 2211 |
Multiple reporting doctors |
|
Multiple sclerosis clinic |
Inflammatory CNS disorders |
Weekly |
9382 2414 |
Prof A. Krishnan |
|
General neurology clinic |
General neurological problems |
Three times a week |
9382 2407, 9382 2422, 9382 2414 |
Profs J Colebatch, A Zagami, A Krishnan, Dr J. Offord, Dr D Dhanapalaratnam |
|
Private clinics |
General neurological problems |
Three times a week |
9382 2407, 9382 2422 |
Profs J Colebatch, A Zagami |
For more information, please see our links on the right hand side of this page.
You need a referral letter from your local general practitioner (GP) or medical practitioner to access this service.
Your doctor will need to fax your referral letter to us to the appropriate fax number. If there is a waiting list, you will receive a confirmation letter and be told what to do next. If there is no waiting list, you will receive a letter providing details on the time and date of your appointment booking or we will contact you to arrange a suitable time. You may receive an SMS or telephone reminder prior to your appointment.
If you need to change or cancel your appointment please telephone the relevant number in our list of clinics. This will allow us to make the time available to another patient.
Please bring:
- Your appointment letter
- Any special items listed on your letter
- TAC or Workcover claim number (if relevant)
- Medicare card
- Health Care Card and/or concession card
- Private health insurance card
- Adverse drug alert card
- Previous x-ray films, scans, ultrasounds or any other test results or reports relevant to your current condition
- Medicines you need to take while you are here
- List of medicines you are currently taking (or the boxes), including medicines you have bought without a prescription, such as herbal supplements and vitamins
- Glasses, hearing aid, walking frame
If you are having a day procedure, please bring:
- Responsible adult carer to stay with you to hear instructions, help you and take you home
- Comfortable day clothes, such as a tracksuit
Please let us know if you need an interpreter. You can contact us telephoning the Translating and Interpreting Service (TIS) on 131 450. Tell the operator what language you speak and then ask the interpreter to set up a telephone conversation between you, an interpreter, and the healthcare professional you want to speak with.
We are teaching hospital and you may be asked to have students present at your appointment or to be involved in research. You have a right to say no. If you do so, this will may cause a slight delay but will not impact on the services we will provide. You may be seen by a senior registrar or Fellow.
Stroke Unit (Acute)
How we can help you
Our Acute Stroke Unit provides care to patients who are being treated and/or investigated for an acute stroke or transient ischaemic attack.
We also have an Acute Stroke emergency response team who work with Emergency Department staff to lead all Acute Stroke calls. They also visit patients in hospital who show any signs of neurological deterioration and potential stroke.
We use the latest medical techniques to remove or dissolve blood clots and restore blood flow to the brain.
We also use a variety of medical imaging techniques to diagnose, treat or prevent strokes. These can include scans of your brain and heart.
The Acute Stroke Unit is one of our Neurology Services.
|
Stroke A stroke is a serious medical emergency that occurs when there is a decrease in the blood supply to your brain and seriously affects its function. Urgent medical attention is required to prevent permanent damage or possibly death. Transient ischaemic attack (TIA) A TIA is when the blood supply to your brain is only temporarily blocked. The signs are the same as a stroke but only last for a few minutes. A TIA is a warning sign that you may have a stroke. If you are worried that you, or your family/friend is having a stroke or TIA, dial 000 immediately and ask for an ambulance.You can find the signs and symptoms for stroke or TIA in this Stroke Foundation information. |
Manager
Nursing Manager Divna Kuzmich
How to find us
Level 8 South, Acute Services Building (building 30 on our campus map)
Information about how to get to our Randwick campus
A range of health professionals will work together to manage your medical treatment, physical and cognitive recovery. We aim to be as collaborative, professional, informative, compassionate and supportive as possible.
Medical Specialists
Professor Alessandro Zagami (Stroke Medical Director)
Professor James Colebatch (Head of Neurology)
Professor Kenneth Butcher (Director of NSW Telestroke)
Professor Arun Krishnan
Dr Michal Lubomski
Dr Julia Thompson
Dr Leon Edwards
Dr Hanka Laue-Gizzi
Dr Christian Zentner
Dr Joanna Offord
Dr Sophie Waller
Medical Team
Advanced Trainee
Medical Registrar
Junior Medical Officers
Nursing Team
Nursing Unit Manager: Divna Kuzmich
Nurse Practitioner: Alanah Bailey
Our nursing team includes a clinical nurse educator, clinical nurse specialists, registered nursing staff and endorsed enrolled nursing staff
Allied Health
Our Speech Pathologist can help you with your ability to speak and to eat and drink safely after a stroke.
Our Physiotherapist will develop an exercise program designed to maximise your strength, balance and mobility.
Our Occupational Therapist will help you to adjust to life after stroke by giving you the confidence and skills to perform daily tasks and learn new skills. They will also organise any equipment you might need for when you go home.
Our Dietitian will help you make changes to your diet to help with any difficulty you might have with eating or drinking.
Our Social Worker will meet with you and your carer/family as soon as possible after the stroke occurs to provide advice on what financial, social and health care support is available. They are also available to provide counselling and emotional support. They can assist with organising accommodation and care for when you leave hospital.
Our Pharmacist will explain what medicines you need to take and when.
Stroke Unit (Acute)
How we can help you
Our Acute Stroke Unit provides care to patients who are being treated and/or investigated for an acute stroke or transient ischaemic attack.
We also have an Acute Stroke emergency response team who work with Emergency Department staff to lead all Acute Stroke calls. They also visit patients in hospital who show any signs of neurological deterioration and potential stroke.
We use the latest medical techniques to remove or dissolve blood clots and restore blood flow to the brain.
We also use a variety of medical imaging techniques to diagnose, treat or prevent strokes. These can include scans of your brain and heart.
The Acute Stroke Unit is one of our Neurology Services.
|
Stroke A stroke is a serious medical emergency that occurs when there is a decrease in the blood supply to your brain and seriously affects its function. Urgent medical attention is required to prevent permanent damage or possibly death. Transient ischaemic attack (TIA) A TIA is when the blood supply to your brain is only temporarily blocked. The signs are the same as a stroke but only last for a few minutes. A TIA is a warning sign that you may have a stroke. If you are worried that you, or your family/friend is having a stroke or TIA, dial 000 immediately and ask for an ambulance.You can find the signs and symptoms for stroke or TIA in this Stroke Foundation information. |
Manager
Nursing Manager Divna Kuzmich
How to find us
Level 8 South, Acute Services Building (building 30 on our campus map)
Information about how to get to our Randwick campus
A range of health professionals will work together to manage your medical treatment, physical and cognitive recovery. We aim to be as collaborative, professional, informative, compassionate and supportive as possible.
Medical Specialists
Professor Alessandro Zagami (Stroke Medical Director)
Professor James Colebatch (Head of Neurology)
Professor Kenneth Butcher (Director of NSW Telestroke)
Professor Arun Krishnan
Dr Michal Lubomski
Dr Julia Thompson
Dr Leon Edwards
Dr Hanka Laue-Gizzi
Dr Christian Zentner
Dr Joanna Offord
Dr Sophie Waller
Medical Team
Advanced Trainee
Medical Registrar
Junior Medical Officers
Nursing Team
Nursing Unit Manager: Divna Kuzmich
Nurse Practitioner: Alanah Bailey
Our nursing team includes a clinical nurse educator, clinical nurse specialists, registered nursing staff and endorsed enrolled nursing staff
Allied Health
Our Speech Pathologist can help you with your ability to speak and to eat and drink safely after a stroke.
Our Physiotherapist will develop an exercise program designed to maximise your strength, balance and mobility.
Our Occupational Therapist will help you to adjust to life after stroke by giving you the confidence and skills to perform daily tasks and learn new skills. They will also organise any equipment you might need for when you go home.
Our Dietitian will help you make changes to your diet to help with any difficulty you might have with eating or drinking.
Our Social Worker will meet with you and your carer/family as soon as possible after the stroke occurs to provide advice on what financial, social and health care support is available. They are also available to provide counselling and emotional support. They can assist with organising accommodation and care for when you leave hospital.
Our Pharmacist will explain what medicines you need to take and when.
Nuclear Medicine and PET Department
How we can help you?
We provide a wide range of Nuclear Medicine tests and therapies for adults and children. As we provide services to the Sydney Children’s Hospital, your child will be in a child-friendly environment and will be looked after by staff who are experienced in looking after children, including administering injections.
Nuclear Medicine and PET imaging involves giving you a very small amount of a radioactive tracer (an injection) and using a special camera to take images of your body. This helps us to determine how well your organs are working and to diagnose a wide range of illnesses, for example heart disease, blood clots in lungs, bone infections, sports injuries, and assessment of cancer. The tests are safe and the imaging is painless.The injected tracer is not iodine-based and allergic reactions are extremely rare.
We are accredited to provide a full range of Nuclear Medicine and PET services and are approved to train Nuclear Medicine Technologists, Specialist Doctors, Physicists and Radiopharmaceutical Scientists.
Some of the more common procedures we perform include:
- Heart scans
- Kidney scans
- Bone scans
- Stomach, bowel, biliary and liver scans
- Lung scans
- Thyroid and parathyroid scans
- Positron Emission Tomography (PET) scans
- Radio-iodine thyroid therapy.
Managers
Medical: Eva Wegner (Head of Department)
Nursing: Min-Ting Pamela Lim (Nurse Unit Manager)
Allied Health: Caryl Christian (Chief Technologist)
Opening hours
7.45am - 4.30pm Monday - Friday
Closed on weekends
How to find us
Level 2, Campus Centre, Prince of Wales Hospital (building 16 in our campus map)
More information about how to get to the Randwick Health Campus

Our Department is staffed by a team of Nuclear Medicine Specialists, Junior Doctors, Nuclear Medicine Technologists, Nurses, Radiopharmaceutical Scientists, Physicists and Clerical Staff.
We work in partnership with your Doctors, The Prince of Wales Hospital and Community Health Services, The Royal Women’s Hospital, The Sydney Children’s Hospital and Sydney/Sydney Eye Hospitals.
You will need a referral letter from a Medical Practitioner (your GP or Specialist) to use our service. The referral needs to include a brief history of your health, what procedure or test they are requesting and why.
You can book an appointment over the phone by calling us on 9382 2200, by fax on 9382 2235, by email on seslhd-powhnm@health.nsw.gov.au or in person at our reception. Please provide your contact number, as we need to call you the day before the scan to confirm your appointment.
We will do our best to schedule your preferred appointment time as soon as possible. In most instances an appointment will be available within a couple of days, however, due to the nature of the tracer that we inject, we may not be able to be completely flexible.
If you need to change or cancel your appointment please telephone us on 9382 2200.
How do I prepare for my test?
Many of our procedures do not require any special preparation, but you will need to fast (not eat or drink) for some scans. In addition, some of the tests need you to have special preparation, for example to stop your regular medication or to take additional medication. We will give you the instructions for your particular scan when we make your booking. Please contact our Department if you are not clear what you will need to do to prepare for your test.
What do I need to bring?
- Your referral letter from your GP or Specialist
- Medicare card
- Health Care Card and/or concession card (if you have one)
- Private Health Insurance card (if applicable/if you want to use it)
- Adverse drug alert card (if you have one)
- Previous X-ray films, CT and MRI films or discs, any other test result or reports related to your current health problem
- Medicines you need to take while you are here
- A list of medicines you are currently taking (or the boxes), including medicines you are taking without a prescription, such as herbal supplements and vitamins
- Glasses, hearing aid, walking frame if you use them
Will I need an injection for my test?
Majority of the scans require an injection of tracer into your vein by using a very small needle (butterfly needle). For more complex scans (for example a heart scan or a PET scan), we will need to place a needle into your vein. Our staff is highly skilled in these injections, including injecting children.
Can I drive after the test?
You are able to drive and go about all your normal activities after the test, unless you have been given any sedatives. If you have been given sedatives you will not be able to drive for 24 hours and must arrange for a responsible adult to take you home after your test.
When will my results be available?
Most of the scans are reported on the same day and your final results are usually available within 24 hours after the completion of your scan. Your results are posted or faxed to your referring doctor. You will need to contact your referring doctor to find out your results.
More information about my PET scan
See these FAQ about your PET Scan
Please let us know if you need an interpreter when you make your booking. You can contact us by telephoning the Translating and Interpreting Service (TIS) on 131 450. Tell the operator what language you speak. You can then ask the interpreter to set up a telephone conversation between you, an interpreter, and our department.
Our department is actively involved in training, education and research. We are a teaching hospital and you may be asked to be involved in research or for a trainee to be present at your appointment. You have a right to say no to participating in any research and to not want any observers. If you do so, this will have no impact in any way on the services we will provide.
Nuclear Medicine and PET Department
How we can help you?
We provide a wide range of Nuclear Medicine tests and therapies for adults and children. As we provide services to the Sydney Children’s Hospital, your child will be in a child-friendly environment and will be looked after by staff who are experienced in looking after children, including administering injections.
Nuclear Medicine and PET imaging involves giving you a very small amount of a radioactive tracer (an injection) and using a special camera to take images of your body. This helps us to determine how well your organs are working and to diagnose a wide range of illnesses, for example heart disease, blood clots in lungs, bone infections, sports injuries, and assessment of cancer. The tests are safe and the imaging is painless.The injected tracer is not iodine-based and allergic reactions are extremely rare.
We are accredited to provide a full range of Nuclear Medicine and PET services and are approved to train Nuclear Medicine Technologists, Specialist Doctors, Physicists and Radiopharmaceutical Scientists.
Some of the more common procedures we perform include:
- Heart scans
- Kidney scans
- Bone scans
- Stomach, bowel, biliary and liver scans
- Lung scans
- Thyroid and parathyroid scans
- Positron Emission Tomography (PET) scans
- Radio-iodine thyroid therapy.
Managers
Medical: Eva Wegner (Head of Department)
Nursing: Min-Ting Pamela Lim (Nurse Unit Manager)
Allied Health: Caryl Christian (Chief Technologist)
Opening hours
7.45am - 4.30pm Monday - Friday
Closed on weekends
How to find us
Level 2, Campus Centre, Prince of Wales Hospital (building 16 in our campus map)
More information about how to get to the Randwick Health Campus

Our Department is staffed by a team of Nuclear Medicine Specialists, Junior Doctors, Nuclear Medicine Technologists, Nurses, Radiopharmaceutical Scientists, Physicists and Clerical Staff.
We work in partnership with your Doctors, The Prince of Wales Hospital and Community Health Services, The Royal Women’s Hospital, The Sydney Children’s Hospital and Sydney/Sydney Eye Hospitals.
You will need a referral letter from a Medical Practitioner (your GP or Specialist) to use our service. The referral needs to include a brief history of your health, what procedure or test they are requesting and why.
You can book an appointment over the phone by calling us on 9382 2200, by fax on 9382 2235, by email on seslhd-powhnm@health.nsw.gov.au or in person at our reception. Please provide your contact number, as we need to call you the day before the scan to confirm your appointment.
We will do our best to schedule your preferred appointment time as soon as possible. In most instances an appointment will be available within a couple of days, however, due to the nature of the tracer that we inject, we may not be able to be completely flexible.
If you need to change or cancel your appointment please telephone us on 9382 2200.
How do I prepare for my test?
Many of our procedures do not require any special preparation, but you will need to fast (not eat or drink) for some scans. In addition, some of the tests need you to have special preparation, for example to stop your regular medication or to take additional medication. We will give you the instructions for your particular scan when we make your booking. Please contact our Department if you are not clear what you will need to do to prepare for your test.
What do I need to bring?
- Your referral letter from your GP or Specialist
- Medicare card
- Health Care Card and/or concession card (if you have one)
- Private Health Insurance card (if applicable/if you want to use it)
- Adverse drug alert card (if you have one)
- Previous X-ray films, CT and MRI films or discs, any other test result or reports related to your current health problem
- Medicines you need to take while you are here
- A list of medicines you are currently taking (or the boxes), including medicines you are taking without a prescription, such as herbal supplements and vitamins
- Glasses, hearing aid, walking frame if you use them
Will I need an injection for my test?
Majority of the scans require an injection of tracer into your vein by using a very small needle (butterfly needle). For more complex scans (for example a heart scan or a PET scan), we will need to place a needle into your vein. Our staff is highly skilled in these injections, including injecting children.
Can I drive after the test?
You are able to drive and go about all your normal activities after the test, unless you have been given any sedatives. If you have been given sedatives you will not be able to drive for 24 hours and must arrange for a responsible adult to take you home after your test.
When will my results be available?
Most of the scans are reported on the same day and your final results are usually available within 24 hours after the completion of your scan. Your results are posted or faxed to your referring doctor. You will need to contact your referring doctor to find out your results.
More information about my PET scan
See these FAQ about your PET Scan
Please let us know if you need an interpreter when you make your booking. You can contact us by telephoning the Translating and Interpreting Service (TIS) on 131 450. Tell the operator what language you speak. You can then ask the interpreter to set up a telephone conversation between you, an interpreter, and our department.
Our department is actively involved in training, education and research. We are a teaching hospital and you may be asked to be involved in research or for a trainee to be present at your appointment. You have a right to say no to participating in any research and to not want any observers. If you do so, this will have no impact in any way on the services we will provide.
Nuclear Medicine and PET Department
How we can help you?
We provide a wide range of Nuclear Medicine tests and therapies for adults and children. As we provide services to the Sydney Children’s Hospital, your child will be in a child-friendly environment and will be looked after by staff who are experienced in looking after children, including administering injections.
Nuclear Medicine and PET imaging involves giving you a very small amount of a radioactive tracer (an injection) and using a special camera to take images of your body. This helps us to determine how well your organs are working and to diagnose a wide range of illnesses, for example heart disease, blood clots in lungs, bone infections, sports injuries, and assessment of cancer. The tests are safe and the imaging is painless.The injected tracer is not iodine-based and allergic reactions are extremely rare.
We are accredited to provide a full range of Nuclear Medicine and PET services and are approved to train Nuclear Medicine Technologists, Specialist Doctors, Physicists and Radiopharmaceutical Scientists.
Some of the more common procedures we perform include:
- Heart scans
- Kidney scans
- Bone scans
- Stomach, bowel, biliary and liver scans
- Lung scans
- Thyroid and parathyroid scans
- Positron Emission Tomography (PET) scans
- Radio-iodine thyroid therapy.
Managers
Medical: Eva Wegner (Head of Department)
Nursing: Min-Ting Pamela Lim (Nurse Unit Manager)
Allied Health: Caryl Christian (Chief Technologist)
Opening hours
7.45am - 4.30pm Monday - Friday
Closed on weekends
How to find us
Level 2, Campus Centre, Prince of Wales Hospital (building 16 in our campus map)
More information about how to get to the Randwick Health Campus

Our Department is staffed by a team of Nuclear Medicine Specialists, Junior Doctors, Nuclear Medicine Technologists, Nurses, Radiopharmaceutical Scientists, Physicists and Clerical Staff.
We work in partnership with your Doctors, The Prince of Wales Hospital and Community Health Services, The Royal Women’s Hospital, The Sydney Children’s Hospital and Sydney/Sydney Eye Hospitals.
You will need a referral letter from a Medical Practitioner (your GP or Specialist) to use our service. The referral needs to include a brief history of your health, what procedure or test they are requesting and why.
You can book an appointment over the phone by calling us on 9382 2200, by fax on 9382 2235, by email on seslhd-powhnm@health.nsw.gov.au or in person at our reception. Please provide your contact number, as we need to call you the day before the scan to confirm your appointment.
We will do our best to schedule your preferred appointment time as soon as possible. In most instances an appointment will be available within a couple of days, however, due to the nature of the tracer that we inject, we may not be able to be completely flexible.
If you need to change or cancel your appointment please telephone us on 9382 2200.
How do I prepare for my test?
Many of our procedures do not require any special preparation, but you will need to fast (not eat or drink) for some scans. In addition, some of the tests need you to have special preparation, for example to stop your regular medication or to take additional medication. We will give you the instructions for your particular scan when we make your booking. Please contact our Department if you are not clear what you will need to do to prepare for your test.
What do I need to bring?
- Your referral letter from your GP or Specialist
- Medicare card
- Health Care Card and/or concession card (if you have one)
- Private Health Insurance card (if applicable/if you want to use it)
- Adverse drug alert card (if you have one)
- Previous X-ray films, CT and MRI films or discs, any other test result or reports related to your current health problem
- Medicines you need to take while you are here
- A list of medicines you are currently taking (or the boxes), including medicines you are taking without a prescription, such as herbal supplements and vitamins
- Glasses, hearing aid, walking frame if you use them
Will I need an injection for my test?
Majority of the scans require an injection of tracer into your vein by using a very small needle (butterfly needle). For more complex scans (for example a heart scan or a PET scan), we will need to place a needle into your vein. Our staff is highly skilled in these injections, including injecting children.
Can I drive after the test?
You are able to drive and go about all your normal activities after the test, unless you have been given any sedatives. If you have been given sedatives you will not be able to drive for 24 hours and must arrange for a responsible adult to take you home after your test.
When will my results be available?
Most of the scans are reported on the same day and your final results are usually available within 24 hours after the completion of your scan. Your results are posted or faxed to your referring doctor. You will need to contact your referring doctor to find out your results.
More information about my PET scan
See these FAQ about your PET Scan
Please let us know if you need an interpreter when you make your booking. You can contact us by telephoning the Translating and Interpreting Service (TIS) on 131 450. Tell the operator what language you speak. You can then ask the interpreter to set up a telephone conversation between you, an interpreter, and our department.
Our department is actively involved in training, education and research. We are a teaching hospital and you may be asked to be involved in research or for a trainee to be present at your appointment. You have a right to say no to participating in any research and to not want any observers. If you do so, this will have no impact in any way on the services we will provide.
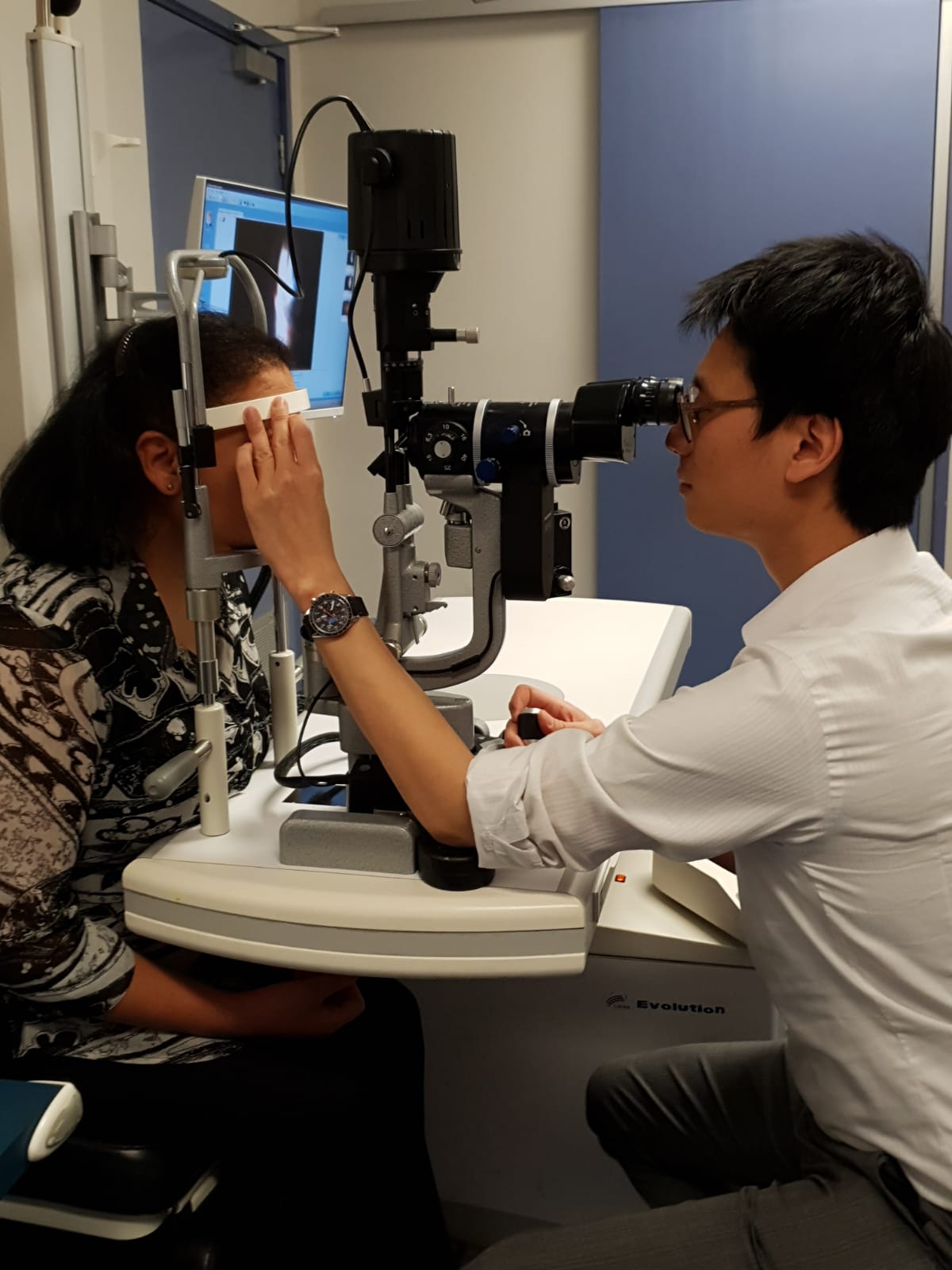
Eye Clinic for Prince of Wales Hospital
How we can help you
The Prince of Wales Hospital Eye Clinic is an outpatient clinic which provides comprehensive medical and surgical ophthalmic and orthoptic care to adults with eye related problems.
The Eye Clinic is located on Level 4, High Street Building, Prince of Wales Hospital.
|
Ophthalmic care is given by our ophthalmologists, specialist doctors who can provide diagnosis, medical treatment and complex microsurgery. Orthoptic care is given by our orthopists, eye health professionals who are trained in assessment, diagnosis and non-surgical treatment of problems with eye movement, squint, double vision and lazy eye. |
The Prince of Wales Eye Clinic provide services for adults with the following eye problems:
- Cataracts
- Diabetic eye disorders
- Glaucoma
- Macular degeneration
- Retinal and vitreous disorders and conditions
- Eye emergency and eye trauma treatment
- Cornea
- Cancer of the eye
- Immunology and inflammation of the middle eye (uveitis)
- Neuro-ophthalmology
- Ophthalmic plastic and orbit surgery
We also provide 24 hours a day, 7 days a week emergency care to the Emergency Department of The Prince of Wales Hospital.
Our Outback Eye Service is based in the Department of Ophthalmology at The Prince of Wales Hospital.
The Sydney Children's Hospital Lion’s Eye Clinic is located in the Sydney Children's Hospital main building on Level 0. It provides assessment and treatment for all aspects of paediatric (ie. children aged 16 years and younger) ophthalmology.
Manager
Nursing Manager Michael Cowan
Opening times
8.00am to 4.30pm Monday to Friday
We are closed on weekends and public holidays.
How to find us
Level 4, High St Building, Prince of Wales Hospital (Building 2 on our campus map)
Information about how to get to our Randwick campus
The eye clinic is staffed by:
- Doctors - Specialist Ophthalmologists, Ophthalmology Registrars and Hospital Resident Medical Officer;
- Ophthalmic Nurses
- Orthoptists
- Technical Officers; and
- Clerical and administrative staff.
We work in partnership with your local general practitioner (GP) and both hospital.
If you are new to the eye clinic and have not previously requested an appointment you must have a referral from your local general practitioner (GP) or Optometrist to use our service. They will prepare a written referral for you, which includes a description of the clinical problem.
Please fax, post in the mail or bring the referral letter to our Eye Clinic.
Once we have received your completed referral you will be placed in a wait-list for the next available appointment. When your appointment has been confirmed, we will send you a letter to your home address confirming the date, time and location of your appointment.
Please make sure your referring GP or Optometrist has your current contact details (particularly your address), otherwise we may not be able to contact you with your appointment.
If you are a current patient, please book a follow up appointment at the Eye Clinic reception after your consultation with our Doctor, prior to leaving.
If we have long waiting times for non-urgent conditions and your need is not urgent (e.g. eye check up for prescription glasses) we may make arrangements for you to visit a different service.
To change or cancel your appointment
If you need to change or cancel your appointment, please contact us as soon as possible on 9382 2261, Monday to Friday 8.00am – 4.30pm.
Changing your appointment may mean we need to place you back on the wait-list. You may need to wait to 8-12 months for your next appointment.
To help us with your request please provide the following information when making your change or cancellation request:
- Your full name
- Your Medicare number
- Date of birth
- Telephone number
- The date and time of your original appointment.
If you cannot attend and do not notify us in advance, you will not be automatically given another appointment at the Eye Clinic. You will need to return to your GP or Optometrist to arrange a new referral and new appointment with us.
If any of your contact details change please let us know by phone on 9382 2261 or in person at the Eye Clinic reception.
Please remember to bring to your appointment:
- A list of your current medicines to your appointment
- Details of any previous reactions to eye drops
- Details of your past medical history
- Current glasses
- Eye related problems and treatments.
You will be unable to drive home if you are having dilating eye drops during your appointment. If this is the case please arrange alternative transport home after your appointment.
Your visit to the Eye Clinic may involve these steps:
1. Check-in
Please go to the Eye Clinic reception to check-in. Our administration staff will confirm that your contact details (in particular your address) are up to date on our records. Please do not arrive earlier than 15 minutes prior to your appointment time.
2. Initial eye assessment
After checking-in, you will be asked to wait in the waiting room for your initial eye assessment.
Your eye assessment may involve various staff (eg. Orthoptists and Ophthalmic nurses), who each have differing roles to play in relation to your eye testing. The relevant staff members will introduce themselves to you by name, and describe their role in your eye assessment.
Each time you meet a new staff member we will ask you about any previous adverse reactions you have had to eye drops (if you needed them). Our staff will also ask you to describe your symptoms and your past medical history and also any eye problems and treatments you have had.
Eye assessments often involve the use of eye drops to determine your eye pressure, or to dilate your pupils so that the internal structure of your eyes can be examined. This can take up to 20 minutes to take effect.
You may need a number of tests and need to wait on the availability of the specialised equipment that we use and the availability of staff to perform these tests for you.
3. Eye consultation
After the eye assessment has been performed, you will be seen by the Ophthalmology Consultant or Registrar doctor to discuss your symptoms and treatment.
4. Booking follow-up appointment (if required)
After meeting with the Ophthalmology Consultant or Registrar doctor you may need to go to the Eye Clinic Reception desk to book a follow-up appointment before leaving the clinic.
5. Going home
We recommend you organise someone else to drive you home. If you are given dilating drops your eyesight can be blurred and you will be more sensitive to light for a few hours.
A visit to our eye clinic can often take several hours. Please do not check-in earlier than 15 minutes prior to your appointment time.
Our services are shared between eye clinic outpatients, hospital inpatients, emergencies in our Emergency Department, operating theatres and other services. We always treat patients on the basis of clinical urgency and at times our medical staff may be called away to attend urgent cases. If there is a delay we will let you know when you check-in. Occasionally, we may need to reschedule your appointment.
We appreciate your patience in circumstances where wait-times are longer than expected.
If you are told you will need to continue to use eye drops after leaving our clinic you will be given an initial supply plus a prescription to get more from your pharmacy. If you need further prescriptions, you will need to organise this with your local GP. We suggest you take an eye drop bottle with you to show them.
Sometimes it can take several weeks before your GP and/or Optometrist (who referred you to the Eye Clinic) receives the letter explaining your visit to our clinic. explaining your diagnosis, treatment plan and follow up arrangements. It is important for you to understand your eye condition, the treatment required, and follow up arrangements prior to leaving our clinic.
If you experience an unexpected or urgent eye problem between appointments, please contact:
- The Eye Clinic on 9382 2261 (Press option 2, then 4), during our opening hours, or
- Your General Practitioner or Optometrist, or
- The nearest Hospital Emergency Department (if an emergency).
Please let us know at least 30 days before your appointment if you need an interpreter. You can contact us telephoning the Translating and Interpreting Service (TIS) on 131 450. Tell the operator what language you speak and then ask the interpreter to set up a telephone conversation between you, an interpreter, and the healthcare professional you want to speak with.
We are teaching hospital and you may be asked to be involved in research or for a student to be present at your appointment. You have a right to say no. If you do so, this will no impact in any way on the services we will provide.
We appreciate your feedback. If you would like to give us feedback on our services please complete a feedback form when you come to an appointment.
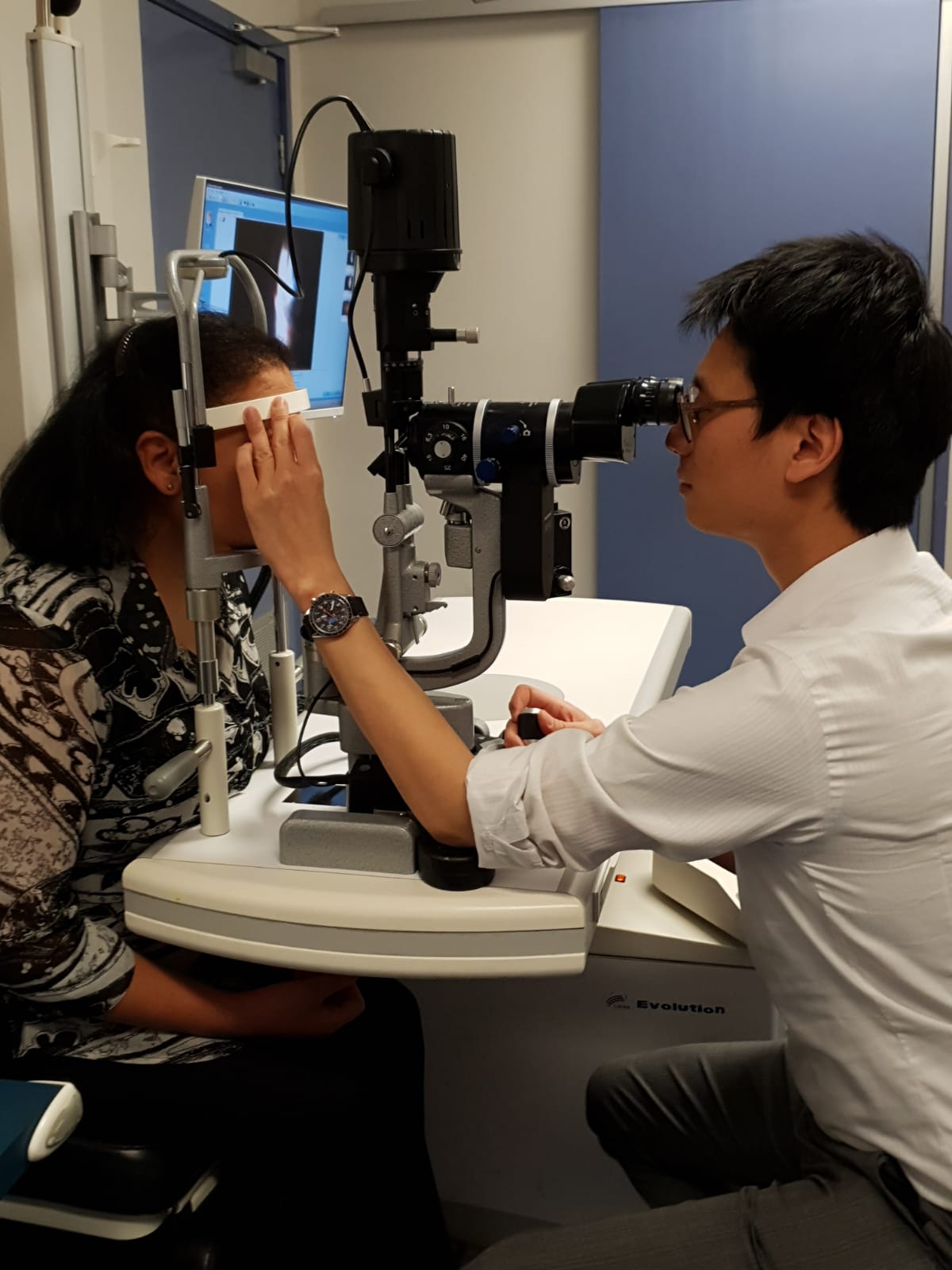
Eye Clinic for Prince of Wales Hospital
How we can help you
The Prince of Wales Hospital Eye Clinic is an outpatient clinic which provides comprehensive medical and surgical ophthalmic and orthoptic care to adults with eye related problems.
The Eye Clinic is located on Level 4, High Street Building, Prince of Wales Hospital.
|
Ophthalmic care is given by our ophthalmologists, specialist doctors who can provide diagnosis, medical treatment and complex microsurgery. Orthoptic care is given by our orthopists, eye health professionals who are trained in assessment, diagnosis and non-surgical treatment of problems with eye movement, squint, double vision and lazy eye. |
The Prince of Wales Eye Clinic provide services for adults with the following eye problems:
- Cataracts
- Diabetic eye disorders
- Glaucoma
- Macular degeneration
- Retinal and vitreous disorders and conditions
- Eye emergency and eye trauma treatment
- Cornea
- Cancer of the eye
- Immunology and inflammation of the middle eye (uveitis)
- Neuro-ophthalmology
- Ophthalmic plastic and orbit surgery
We also provide 24 hours a day, 7 days a week emergency care to the Emergency Department of The Prince of Wales Hospital.
Our Outback Eye Service is based in the Department of Ophthalmology at The Prince of Wales Hospital.
The Sydney Children's Hospital Lion’s Eye Clinic is located in the Sydney Children's Hospital main building on Level 0. It provides assessment and treatment for all aspects of paediatric (ie. children aged 16 years and younger) ophthalmology.
Manager
Nursing Manager Michael Cowan
Opening times
8.00am to 4.30pm Monday to Friday
We are closed on weekends and public holidays.
How to find us
Level 4, High St Building, Prince of Wales Hospital (Building 2 on our campus map)
Information about how to get to our Randwick campus
The eye clinic is staffed by:
- Doctors - Specialist Ophthalmologists, Ophthalmology Registrars and Hospital Resident Medical Officer;
- Ophthalmic Nurses
- Orthoptists
- Technical Officers; and
- Clerical and administrative staff.
We work in partnership with your local general practitioner (GP) and both hospital.
If you are new to the eye clinic and have not previously requested an appointment you must have a referral from your local general practitioner (GP) or Optometrist to use our service. They will prepare a written referral for you, which includes a description of the clinical problem.
Please fax, post in the mail or bring the referral letter to our Eye Clinic.
Once we have received your completed referral you will be placed in a wait-list for the next available appointment. When your appointment has been confirmed, we will send you a letter to your home address confirming the date, time and location of your appointment.
Please make sure your referring GP or Optometrist has your current contact details (particularly your address), otherwise we may not be able to contact you with your appointment.
If you are a current patient, please book a follow up appointment at the Eye Clinic reception after your consultation with our Doctor, prior to leaving.
If we have long waiting times for non-urgent conditions and your need is not urgent (e.g. eye check up for prescription glasses) we may make arrangements for you to visit a different service.
To change or cancel your appointment
If you need to change or cancel your appointment, please contact us as soon as possible on 9382 2261, Monday to Friday 8.00am – 4.30pm.
Changing your appointment may mean we need to place you back on the wait-list. You may need to wait to 8-12 months for your next appointment.
To help us with your request please provide the following information when making your change or cancellation request:
- Your full name
- Your Medicare number
- Date of birth
- Telephone number
- The date and time of your original appointment.
If you cannot attend and do not notify us in advance, you will not be automatically given another appointment at the Eye Clinic. You will need to return to your GP or Optometrist to arrange a new referral and new appointment with us.
If any of your contact details change please let us know by phone on 9382 2261 or in person at the Eye Clinic reception.
Please remember to bring to your appointment:
- A list of your current medicines to your appointment
- Details of any previous reactions to eye drops
- Details of your past medical history
- Current glasses
- Eye related problems and treatments.
You will be unable to drive home if you are having dilating eye drops during your appointment. If this is the case please arrange alternative transport home after your appointment.
Your visit to the Eye Clinic may involve these steps:
1. Check-in
Please go to the Eye Clinic reception to check-in. Our administration staff will confirm that your contact details (in particular your address) are up to date on our records. Please do not arrive earlier than 15 minutes prior to your appointment time.
2. Initial eye assessment
After checking-in, you will be asked to wait in the waiting room for your initial eye assessment.
Your eye assessment may involve various staff (eg. Orthoptists and Ophthalmic nurses), who each have differing roles to play in relation to your eye testing. The relevant staff members will introduce themselves to you by name, and describe their role in your eye assessment.
Each time you meet a new staff member we will ask you about any previous adverse reactions you have had to eye drops (if you needed them). Our staff will also ask you to describe your symptoms and your past medical history and also any eye problems and treatments you have had.
Eye assessments often involve the use of eye drops to determine your eye pressure, or to dilate your pupils so that the internal structure of your eyes can be examined. This can take up to 20 minutes to take effect.
You may need a number of tests and need to wait on the availability of the specialised equipment that we use and the availability of staff to perform these tests for you.
3. Eye consultation
After the eye assessment has been performed, you will be seen by the Ophthalmology Consultant or Registrar doctor to discuss your symptoms and treatment.
4. Booking follow-up appointment (if required)
After meeting with the Ophthalmology Consultant or Registrar doctor you may need to go to the Eye Clinic Reception desk to book a follow-up appointment before leaving the clinic.
5. Going home
We recommend you organise someone else to drive you home. If you are given dilating drops your eyesight can be blurred and you will be more sensitive to light for a few hours.
A visit to our eye clinic can often take several hours. Please do not check-in earlier than 15 minutes prior to your appointment time.
Our services are shared between eye clinic outpatients, hospital inpatients, emergencies in our Emergency Department, operating theatres and other services. We always treat patients on the basis of clinical urgency and at times our medical staff may be called away to attend urgent cases. If there is a delay we will let you know when you check-in. Occasionally, we may need to reschedule your appointment.
We appreciate your patience in circumstances where wait-times are longer than expected.
If you are told you will need to continue to use eye drops after leaving our clinic you will be given an initial supply plus a prescription to get more from your pharmacy. If you need further prescriptions, you will need to organise this with your local GP. We suggest you take an eye drop bottle with you to show them.
Sometimes it can take several weeks before your GP and/or Optometrist (who referred you to the Eye Clinic) receives the letter explaining your visit to our clinic. explaining your diagnosis, treatment plan and follow up arrangements. It is important for you to understand your eye condition, the treatment required, and follow up arrangements prior to leaving our clinic.
If you experience an unexpected or urgent eye problem between appointments, please contact:
- The Eye Clinic on 9382 2261 (Press option 2, then 4), during our opening hours, or
- Your General Practitioner or Optometrist, or
- The nearest Hospital Emergency Department (if an emergency).
Please let us know at least 30 days before your appointment if you need an interpreter. You can contact us telephoning the Translating and Interpreting Service (TIS) on 131 450. Tell the operator what language you speak and then ask the interpreter to set up a telephone conversation between you, an interpreter, and the healthcare professional you want to speak with.
We are teaching hospital and you may be asked to be involved in research or for a student to be present at your appointment. You have a right to say no. If you do so, this will no impact in any way on the services we will provide.
We appreciate your feedback. If you would like to give us feedback on our services please complete a feedback form when you come to an appointment.