The Model for Improvement
South Eastern Sydney Local Health District (SESLHD) uses The Model for Improvement to guide improvement work.
The Model for Improvement provides a method for structuring an improvement project. It is a simple yet powerful tool for accelerating improvement that is used around the world. The model consists of two parts:
1. The Three Fundamental Questions for Improvement
Before an improvement team begin making changes they need to do some planning. The three fundamental questions for improvement help us to define what we want to achieve, what ideas we think might make a difference and what we’ll measure to help us to understand if change is an improvement.
2. PDSA cycles
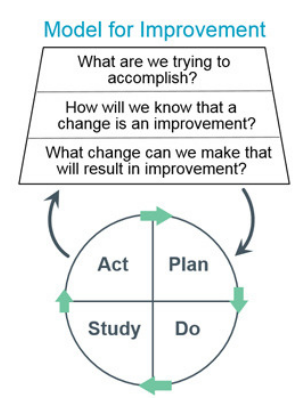 PDSA (Plan Do Study Act) cycles provide the method for the testing of ideas. The cyclical nature allows the change to be refined and improved through repeated cycles of testing and learning.
PDSA (Plan Do Study Act) cycles provide the method for the testing of ideas. The cyclical nature allows the change to be refined and improved through repeated cycles of testing and learning.
You can learn more about The Model for Improvement by watching these whiteboard videos developed by The Institute for Health Improvement:
Aim Statements
One of the first tasks of an improvement team is to set a clear goal to work towards. This goal is reflected as an aim statement that provides an explicit description of the team’s desired outcomes. It addresses what will be improved, by when and by how much.
Agreement on the aim statement will be more easily achieved if team members are provided with relevant information about the current situation i.e. baseline data about the process being investigated.
Examples of aim statements are provided below:
- Reduce the number of unnecessary urine cultures ordered for catheterised patients by 30% before 1 September, 2019
- Within 1 year, 90% of patients suitable for discharge, will be discharged from the ward before 10am
- Within 12 months, decrease the rate of infections in joint replacement surgery to less than 1%
- Within 8 months, decrease the number of admissions with a primary diagnosis of asthma by 50%
- Within 3 months, a catheter removal order will be documented in the medical record of 80% of catheterised patients
- Decrease the number of surgical postponements by 50% by December 2019.
Family of Measures
Once we are clear about what we want to achieve, the next task is to develop a measurement plan.
Health care systems are highly complex and no single measure is adequate in determining success. Multiple measures are required to evaluate the impact of changes. Typically efforts will require a family of measures comprised of three different kinds:
Outcome Measures represent effect of the system on the patient or stakeholder: How is the system performing? What is the result?
Outcome measures are directly linked to your aim e.g. If your project is focusing on falls reduction then your outcome measure could be the number of falls occurring. There is often a tangible link between the outcome measure and the patient.
Examples include:
- For surgery: Surgical site infection rate
- For diabetes: Average HbA1c level for population of patients with diabetes
- For access: Number of days to 3rd next available appointment
- For critical care: Intensive Care Unit (ICU) percent unadjusted mortality
- For medication systems: Adverse drug events per 1,000 doses
Process Measures relate to the workings of the system that contribute to the intended outcome: Are the parts/steps in the system performing as planned?
Your improvement project will likely involve changing or modifying different processes or systems to hopefully improve the issue you’ve identified. It’s important to measure the reliability of these processes so you can track them back against your aim. For example going back to your falls project, you may want to focus on the process of risk assessment which will then help reduce the number of falls.
Examples include:
- For surgery: Proportion of patient receive antibiotics pre-surgery
- For diabetes: Percentage of patients whose HbA1c level was measured twice in the past year
- For access: Average daily clinician hours available for appointments
- For critical care: Percent of patients with intentional rounding completed on schedule.
Balancing Measures look at a system from different dimensions, considering impact elsewhere: What happened to the system as we improved the outcome and process measures? Were there unanticipated consequences? Balancing measures can help show whether unintended consequences have been introduced elsewhere in the system.
Examples include:
- For surgery: Antibiotics not ceased in a timely way
- For reducing time patients spend on a ventilator after surgery: Make sure re-intubation rates are not increasing
- For reducing patients’ length of stay in the hospital: Make sure readmission rates are not increasing.
Improvement teams should aim to collect between 5-8 key measures that they track over the life of the improvement project. The more frequently this is collected the more feedback they will receive on whether the ideas being tested are impacting on the aim.
Plan-Do-Study-Act (PDSA) Cycle
In order to improve processes we need to make changes although not every change will result in improvement. What is best practice? What evidence do you have from elsewhere about what is most likely to work? What do you and your team think will work? What have other people done that you could try?
This is an opportunity for the team to develop ideas for testing. If there is a clear evidence base then you need to use this. However, in cases where this does not exist then you can use creative thinking techniques to generate ideas for testing.. Once you have a clear idea of what you would like to test out as a team use PDSA cycles, which allow you to test the change in the workplace setting
Remember that you know your own system best, so keep your objectives in mind and use your knowledge and experience to guide you.
The second part of the Model for Improvement is effectively your engine for developing, testing and implementing changes. This is carried out by using Plan, Do, Study, Act (PDSA) cycles.
| Act | Plan |
|
|
| Study | Do |
|
|
PDSA cycles allow you to take change ideas you have created, try them in practice, learn what is or isn’t working with them and then adjust your approach. It is rare to achieve absolute success through your first PDSA cycle. Most commonly you will need to adjust your change idea through a number of PDSA cycles before it starts to work reliably in actual practice. The important point to note is that failure is not the end and can be a useful thing! By meeting on a regular basis as a team and going through PDSA cycles you will be doing something called rapid cycle testing. This will allow you to see meaningful change within months that would otherwise take years.
